
The subject of tooth resorption (TR) may be unsettling to even the most seasoned dental practitioner. TR is also known as:
The American Veterinary Dental College (AVDC) now classifies this condition simply as “tooth resorption,” with five progressive stages based on the severity of the lesion, and three types based on the location (root, crown, or both). Internal resorption is a further descriptor for when the process of resorption of the dental hard tissue begins from within the pulp cavity. Visit AVDC to view stages of tooth resorption.
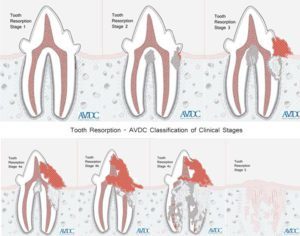
Copyright© AVDC®, used with permission
TR has been reported in multiple species and is definitely seen in dogs and cats. It is the second most common feline dental problem (after periodontal disease) and it has been reported that up to 75% of cats will experience at least one TR in their lifetime. There is no minimum age of onset for this disease, but it is most common in middle-aged to geriatric animals. When TR is present above the gumline, this condition is very painful as sensitive dentin, granulation tissue, or even the pulp may be exposed. Below the gumline, lost tooth structure is replaced with bone. TR in any location can also weaken the tooth, causing fracture or complete loss of the crown. Root resorption, which can cause ankylosis in dogs and may be common as they age, can cause loss of the “shock absorber” properties of the periodontal ligament. This can then predispose the tooth to chip or break if the pet chews on something too hard (even if they’ve never had a problem with it before).
The full etiology of TR is still not well-understood, but inflammation appears to play a role. What we do know is that odontoclasts, which are responsible for the normal remodeling of the tooth, become activated and not appropriately regulated or turned off. An analogy might be osteoclasts in the case of osteoporosis. Much research is ongoing as to the causes of this activation and possible treatments. It has been proposed that there is a genetic component to the condition, and TR appears to be more common in pure-bred cats. If an animal has one affected tooth, then they are more likely to have more teeth affected in the future.

A double-ended periodontal probe (with millimeter markings) and shepherd’s hook explorer by Cislak. This instrument is used for a complete oral exam in every patient.
This knowledge is based on clinical observation as well as extrapolation from TR in humans. However, TR below the gumline may compromise the blood supply to the tooth, and it can become non-vital. Additionally, the progression of these lesions can occur quickly, especially in cats, so care must be taken not to neglect any teeth that may become a problem in the near future.
Some TR can be diagnosed with visual and tactile examination. Sometimes the lesions are obvious, even in the awake patient; however, it must be differentiated from things such as an oral mass, gingival hyperplasia, or simply gingivitis. A delicate shepherd’s hook explorer is the best tool for probing each tooth; used at a 90° angle to the tooth at the gumline on all sides (buccal, palatal/lingual, mesial, and distal aspects), it is sensitive enough to pick up even the smallest lesions invisible to the naked eye. The tool may make a distinct sound when it catches on a defect; this must be differentiated from simply catching on a normal part of the tooth that may be exposed with periodontal disease. Of course, this probing should be done when calculus has been removed so no lesions are missed. Calculus will often build up over TR lesions because the animal avoids chewing with that due to pain. Removal of this calculus re-exposes the sensitive tissue, and if the TR is not addressed, it may be more painful than it was when it was covered in calculus. Probing these lesions will often elicit a painful response, such as chattering, even under a surgical plane of anesthesia.
At this time, extraction is the only known treatment for TR. This removes the source of pain and prevents the tooth from being further compromised. In the past, when we thought of these lesions like caries, some practitioners would treat them as such with composite restoration. Because that does not address the underlying cause, the condition progresses, and within a few months, the filling will fall out, and the tooth will be painful again.
Dental radiographs may not always be necessary in diagnosing clinical tooth resorption when evident above the gumline, but they are essential for planning treatment. While the stage and type of TR may be academic, knowing what the root structure looks like (or in cases of advanced TR, where the crown is already lost, knowing if any root structure is left) is imperative. Often these extractions require larger gingival flaps and removal of more alveolar bone than a standard extraction. Ankylosis, or fusion of the tooth root to the alveolar bone, is a major cause for breaking a tooth during extraction and causing retained tooth roots.
Crown amputation is one described therapy for treating these teeth. It involves simply removing the crown, smoothing the alveolar bone at the gumline, and closing the gingiva over the bone. However, crown amputation is only appropriate in certain cases, and dental radiographs must be available to evaluate this. All of the following criteria for crown amputation must be present; they are:
In multi-rooted teeth, it may be appropriate to extract one root and crown amputate another. Care must be taken when extracting teeth with TR because complications such as retained tooth roots, translocation of roots (eg. pushing a root into the mandibular canal or nasal cavity), or iatrogenic jaw fracture may be more likely to occur due to the difficulty of these extractions. Pain medication should be prescribed and continued until the tooth has been treated if extraction cannot be performed at the time of diagnosis.
"There is no known prevention for TR. No diet, home care, or product, such as fluoride, has been shown to have any benefit for this condition."
Annual (or semi-annual) anesthetized oral exams and dental radiographs are recommended for all animals to screen for TR. Once a patient has been diagnosed with TR on at least one tooth, the other teeth should be carefully evaluated regularly. Even if TR is only present below the gumline, that tooth must be monitored for progression into the crown.
Tooth resorption can be extremely frustrating for client and practitioner. Myself and Dr. Duncan are always available to help with any questions or case consults you may have.
Happy Pet Dental Health Month!